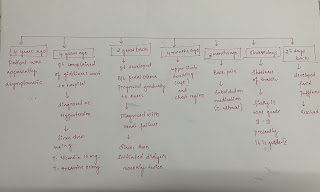
thrombocytopenia and pyrexia in 52 year old male
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This E log book also reflects my patient-centered online learning portfolio.
Case:
A 52 year old male who is a toddy collector by occupation and resident of Nalgonda came to OPD on 8/6/22 with the chief complaints of fever since 4 days,
decreased appetite since 3days,
tightness of abdomen since 3days.
History of present illness:
-Patient was apparently asymptomatic 4 days ago. He then developed fever of low grade, sudden in onset, gradually progressive and relieved on medication.
-He also had complaints of abdominal distension which was gradual and progressive in nature. It is associated with pain. Abdominal pain aggravated on intake of liquids, solids.
- abdominal tightness is also present.
-Patient then approached local RMP and was given medication for 4 days. But symptoms recurred the next day.
No history of rashes ,bleeding tendencies
No history of headache ,vomitings, generalised body pains
No history of loose stools , pain abdomen
No history of weight loss
Past history-
Not a k/c/o DM ,HTN, TB,ASTHMA,cva, cad
Personal history :
Diet :mixed
Appetite : normal
Sleep : adequate
Bowel and bladder movements:regular
Occasional alcoholic & toddy intake
Family history :
Not significant
General examination:
Patient is consious, coherent, cooperative.
No signs of icterus, pallor,clubbing, lymphadenopathy, edema.
Vitals:
Temp: 98.6 F
PR: 84 bpm
RR: 20 cpm
Grbs: 115 mg/dl
Spo2: 98%
Systemic examination
Per Abdomen
Inspection:
Skin - smooth (scar from childhood)
Shape - distended
Umbilicus - normal
Abdominal wall movements - present
No visible pulsations and peristaltic movements seen.
Palpation:
Tenderness - mild
No rise of temperature
Liver - not palpable
Spleen - mild palpable
Gall bladder - not palpable
Kidneys - not palpable
Percussion:
Liver - dull note
Spleen - dull note
No shifting dullness, fluid thrill.
Auscultation:
Bowel sounds heard.
No bruit.
CARDIOVASCULAR SYSTEM-
Inspection-
The chest wall is bilaterally symmetrical.
No dilated veins, scars or sinuses are seen
Apical impulse or pulsations can be appreciated in sixth intercostal space 2cms lateral to mid clavicular line
Palpation-
Apical impulse is felt in the sixth intercostal space, 2 cm away from the midclavicular line
No parasternal heave or thrills are felt
Percussion-
Right and left borders of the heart are percussed
Auscultation-
S1 and S2 heard, no added thrills and murmurs are heard
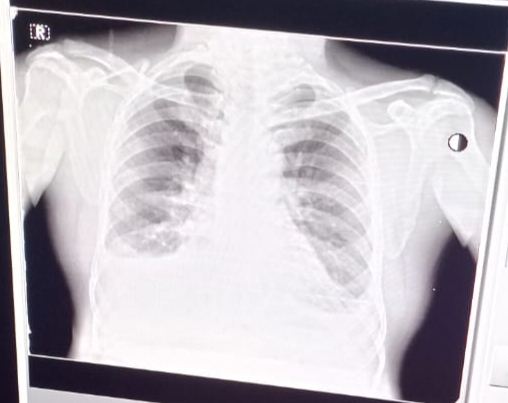
RESPIRATORY SYSTEM-
Inspection-
Chest is bilaterally symmetrical
The trachea is positioned centrally
Apical impulse is not appreciated
Chest moves normally with respiration
No dilated veins, scars or sinuses are seen
Palpation-
Trachea is felt in the midline
Chest moves equally on both sides
Apical impulse is felt in the sixth intercostal space
Tactile vocal fremitus- appreciated
Percussion-
The areas percussed include the supraclavicular, infraclavicular, mammary, axillary, infraaxillary, suprascapular, infrascapular areas.
They are all resonant.
Auscultation-
Normal vesicular breath sounds are heard
Central nervous system:
No abnormalities detected
INVESTIGATIONS
Hemogram:
Hb-14.9
TLC-10,500
N-43
L-48
E-01
RBC-5.02
PLT-22,000
Blood urea-59
Serum creatinine-1.6
Serum Electrolytes-
Na+ :141
K+ :3.9
Cl- :103
LFT
Total bilirubin -1.27
Direct bilirubin -0.44
SGOT-60
SGPT-47
ALP-127
Total protein-5.9
Albumin-3.5
A/G ratio-1.48
CUE
ALbumin- ++
Pus cells -4.6
Epithelial cells:2-3
USG :
Fatty liver (grade 2)
Mild splenomegaly
Mild pleural effusion in right lungs
Provisional diagnosis:
-viral pyrexia with thrombocytopenia
O/E :
Pt is conscious,coherent ,cooperative
Temp: 103 F
Bp: 120/ 70mmhg
Pr: 90 bpm
RR: 24 cpm
SYSTEMIC EXAMINATION:
CVS:
S1, S2 heard. No murmurs heard.
RS:
Bilateral air entry present
Per abdomen:
Soft, mild tenderness
Shape: distended
Bowel sounds heard.
Treatment
On 13th
Oral fluids
Tab dolo 650 mg/po/sos
Tab pan 40 mg
Doxycycline 100 mg
Zincovit
8th hourly monitoring of vitals

Comments
Post a Comment