This is the link of the questions asked regarding the cases:
http://medicinedepartment.blogspot.com/2021/05/online-blended-bimonthly-assignment.html?m=1
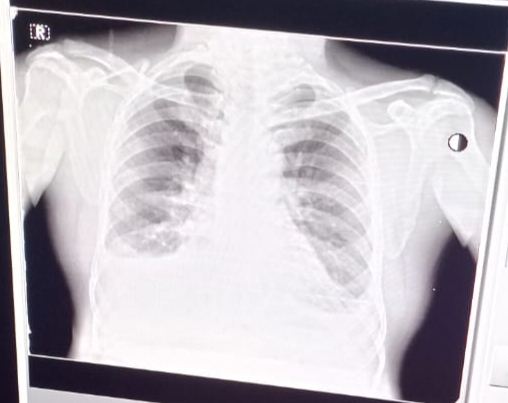
1) PULMONOLOGY
https://soumyanadella128eloggm.blogspot.com/2021/05/a-55-year-old-female-with-shortness-of.html
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
ANSWER
evolution of symptomatology of the patient can be
evolution of symptomatology of the patient can be
exposure to bacteria/virus/or change in the quality of air ( as she worked in paddy fields during the month of January)leading to acute shortness of breath.these symptoms have been relieved by use of brocodialators oral glucocorticoids and antibiotics AS EXACERBATION AND CO MORBIDITIES CONTRIBUTE TO OVERALL SEVERITY OF THE PATIENT ( using indoor chulha for the pass 20 year ) So this can lead to BRONCHIECTASIS which can lead to RIGHT HEART FAILURE. Because of right heart failure which leads to SALT AND WATER RETENTION caused due to renal hypoxia and hypercapnia and this leads to pitting oedema and progressively to HYPERTENSION. DM may be caused due to use of glucocorticoids now and then
ANATOMICAL LOCALIZATION
persistent and preventable sir flow limitation and dilatation of bronchi
ETIOLOGY
indoor chulha for 20 year and working in paddy fields during winter month (january)
indoor chulha for 20 year and working in paddy fields during winter month (january)
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
ANSWER
mechanism of action of the drugs used
AUGMENTIN antibiotic
AZITHROMYCIN antibiotic
the above two drugs are used to teart the lung infection
LASIX is an diuritic used as
Furosemide works by blocking the absorption of sodium, chloride, and water from the filtered fluid in the kidney tubules, causing a profound increase in the output of urine (diuresis)
PANTOP
The mechanism of action of pantoprazole is to inhibit the final step in gastric acid production. In the gastric parietal cell of the stomach, pantoprazole covalently binds to the H+/K+ ATP pump to inhibit gastric acid and basal acid secretion. The covalent binding prevents acid secretion for up to 24 hours and longer.
4. Could the ATT have affected her symptoms? If so how?
ANSWER
mostly no because she has used it for a shorter time
5.What could be the causes for her electrolyte imbalance
ANSWER
It is mainly due to sodium retention in the body due to right heart failure which leads to SALT AND WATER RETENTION caused due to renal hypoxia and hypercapnia
2) Neurology (10 Marks)
https://143vibhahegde.blogspot.com/2021/05/wernickes-encephalopathy.html
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
ANSWER
due to chronic consumption of alcohol patient has developed VITAMIN B12 deficiency alcohol inhibiting a person's ability to fully absorb the necessary nutrients from their food. Cells struggling to uptake this vitamin.which leads to degeneration of nerves mainly mamillary bodies, dorsomedial nuclei of thalamus and periventricular grey matter
function of
1) mamillary body - recollective memory
2)thalamus - it is a relaying of sensory singls and motor signals to cerebral cortex and also responsible for regulation of sleep consciousness and alertness
therefore all the above functions will be altered
ANATOMICAL LOCALIZATION
nervous system
ETIOLOGY
ANATOMICAL LOCALIZATION
nervous system
ETIOLOGY
chronic alcohol consumption
4) What is the reason for giving thiamine in this patient?
ANSWER
due to vitamin B12 deficiency
5) What is the probable reason for kidney injury in this patient?
ANSWER
as the urea levels are every high it denotes an acute renal failure.As high serum creatinine and urea levels are present denotes that reabsorption from tubules is taking place therefore the primary cause is prerenal most probably due to generalized dehydration. A slightly high FENa level also denotes that tubular necrosis is occurring to some degree hence prerenal AKI is in turn leading to ATN
6). What is the probable cause for the normocytic anemia?
ANSWER
may be due to loss of blood through ulcer
may be due to due to renal failure EPO production is reduced
7) Could chronic alcoholism have aggravated the foot ulcer formation? If yes, how and why?
ANSWER
may be dure to ALCOHOLIC NEUROPATHY
https://kausalyavarma.blogspot.com/2021/05/a-52-year-old-male-with-cerebellar.html?m=1
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
ANSWER
ANATOMICAL LOCATION infract in the inferior cerebellar hemishere
ETIOLOGY ataxia is lack of muscle co ordination or control of voluntary movements due to damage of cerebellar
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
ANSWER
VERTIN-BETAHISTINE an anti vertigo
is betahistine, which is an anti- vertigo medication
MOA- It is a weak agonist on H1 receptors located on blood vessels of the inner ear. This
leads to local vasodilation and increased vessel permeability. This can reverse the
underlying problem.
Indications- Prescribed for balance disorders. In this case it is used due to patients
history of giddiness and balance issues.
B) Tab Zofer 4mg- This is ondanseteron- It is an anti emetic
MOA- It is a 5H3 receptor antagonist on vagal afferents in the gut and they block
receptors even in the CTZ and solitary tract nucleus.
Indications- Used to control the episodes of vomiting and nausea in this patient.
C) Tab Ecosprin 75mg- This is aspirin. It is an NSAID
MOA- They inhibit COX-1 and COX-2 thus decreasing the prostaglandin level and
thromboxane synthesis
Indications- They are anti platelet medications and in this case used to prevent
formation of blood clots in blood vessels and prevent stroke.
D) Tab Atorvostatin 40mg- This is a statin
MOA- It is an HMG CoA reductase inhibitor and thus inhibits the rate limiting step in
cholesterol biosynthesis. It decreases blood LDL and VLDL, decreases cholesterol
synthesis, thus increasing LDL receptors in liver and increasing LDL uptake and
degeneration. Hence plasma LDL level decreases.
Indications- Used to treat primary hyperlipidemias. In this case it is used for primary
prevention of stroke.
E) Clopidogrel 75mg- It is an antiplatelet medication
MOA- It inhibits ADP mediated platelet aggregation by blocking P2Y12 receptor on the
platelets.
Indications- In this case it decreases the risk of heart disease and stroke by preventing
clotting
F) Thiamine- It is vitamin B1
It is naturally found in many foods in the human diet. In this case, the patient consumes
excess alcohol- so he may get thiamine deficiency due to poor nutrition and lack of
essential vitamins due to impaired ability of the body to absorb these vitamins.
Indications- Given to this patient mainly to prevent Wernickes encephalopathy- that can
lead to confusion, ataxia and opthalmoplegia.
G) Tab MVT- This is methylcobalamin
Mainly given in this case for vitamin B12 deficiency.
3) Did the patients history of denovo HTN contribute to his current condition?
ANSWER
4) Does the patients history of alcoholism make him more susceptible to ischaemic or haemorrhagic type of stroke?
YES
https://rishikoundinya.blogspot.com/2021/05/55years-old-patient-with-seizures.html
1. Is there any relationship between occurrence of seizure to brain stroke. If yes what is the mechanism behind it?
ANSWER
a stoke causes brain injury. this injury leads scar formation which will effect the electrical activity which may lead to seizure
2. In the previous episodes of seizures, patient didn't loose his consciousness but in the recent episode he lost his consciousness what might be the reason?
ANSWERS
grand mal seizures causes loss of consciousness
https://shivanireddymedicalcasediscussion.blogspot.com/2021/05/a-30-yr-old-male-patient-with-weakness.html
1.Does the patient's history of road traffic accident have any role in his present condition?
ANSWER
NO it was due to alcohol consumption and emotional disturbance
2.What are warning signs of CVA?
ANSWER
difficulty in walking
dizziness
numbness
blurred vision
3.What is the drug rationale in CVA?
ANSWER
Mannitol
Ecospirin
Atorvas
bp monitoring
4. Does alcohol has any role in his attack?
ANSWER
yes
5.Does his lipid profile has any role for his attack??
ANSWER
NO as his lipid profile is normal
https://amishajaiswal03eloggm.blogspot.com/2021/05/a-50-year-old-patient-with-cervical.html
)What is myelopathy hand ?
ANSWER
a)There is loss of power of adduction and extension of the ulnar two or three fingers and an inability to grip and release rapidly with these fingers. These changes have been termed "myelopathy hand" and appear to be due to pyramidal tract involvement.
2)What is finger escape ?
ANSWER
Finger escape
Wartenberg's sign is a neurological sign consisting of involuntary abduction of the fifth (little) finger, caused by unopposed action of the extensor digiti minimi. . This finding of weak finger adduction in cervical myelopathy is also called the "finger escape sign"
3)What is Hoffman’s reflex?
ANSWER
c)
Hoffman's sign or reflex is a test used to examine the reflexes of the upper extremities. This test is a quick, equipment-free way to test for the possible existence of spinal cord compression from a lesion on the spinal cord or another underlying nerve condition
https://neerajareddysingur.blogspot.com/2021/05/general-medicine-case-discussion.html?m=1
1) What can be the cause of her condition ?
ANSWER
According to MRI cortical vein thrombosis might be the cause of her seizures.
2) What are the risk factors for cortical vein thrombosis?
ANSWER
Infections:
Meningitis, otitis,mastoiditis
Prothrombotic states:
Pregnancy, puerperium,antithrombin deficiency proteinc and protein s deficiency,Hormone replacement therapy.
Mechanical:
Head trauma,lumbar puncture
Inflammatory:
SLE,sarcoidosis,Inflammatory bowel disease.
Malignancy.
Dehydration
Nephrotic syndrome
Drugs:
Oral contraceptives,steroids,
Chemotherapy:Cyclosporine and l asparginase
Hematological:
Myeloproliferative Malignancies
Primary and secondary polycythemia
Intracranial :
Dural fistula,
venous anomalies
Vasculitis:
Behcets disease wegeners granulomatosis
3)There was seizure free period in between but again sudden episode of GTCS why?resolved spontaneously why?
ANSWER
Seizures are resolved and seizure free period got achieved after medical intervention but sudden episode of seizure was may be due to any persistence of excitable foci by abnormal firing of neurons.
4) What drug was used in suspicion of cortical venous sinus thrombosis?
ANSWER
Anticoagulants are used for the prevention of harmful blood clots.
Clexane ( enoxaparin) low molecular weight heparin binds and potentiates antithrombin three a serine protease Inhibitor to form complex and irreversibly inactivates factor xa.
3) Cardiology (10 Marks)
A) Link to patient details:
1.What is the difference btw heart failure with preserved ejection fraction and with reduced ejection fraction?
Ans:Preserved ejection fraction (HFpEF) – also referred to as diastolic heart failure. The heart muscle contracts normally but the ventricles do not relax as they should during ventricular filling (or when the ventricles relax).
Reduced ejection fraction (HFrEF) – also referred to as systolic heart failure
HFpEF is preceded by chronic comorbidities, such as hypertension, type 2 diabetes mellitus (T2DM), obesity, and renal insufficiency, whereas HFrEF is often preceded by the acute or chronic loss of cardiomyocytes due to ischemia, a genetic mutation, myocarditis, or valvular disease
2.Why haven't we done pericardiocenetis in this pateint?
Ans: Pericardiocentesis is not done here Because the effusion was self healing ,It reduced from 2.4cm to 1.9 cm.
3.What are the risk factors for development of heart failure in the patient?
Ans: risk factors for development of heart faliure in this patent
Alcohol abuse increases the risk of atrial fibrillation, heart attack and congestive heart failure
high blood pressure
Smoking
Diabetes
AV block can be associated with severe bradycardia and hemodynamic instability. It has a greater risk of progressing to third-degree (complete) heart block or asystole.
wosening of pericardial effusion leaing to cardiac tamponade.
4.What could be the cause for hypotension in this
Ans : visceral pericardium may have thickened which is restricting the heart to expand causing hypotension
(May be secondary to TB)
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
Ans: *the anatomical site is BLOOD VESSELS;
* ETIOLOGY:
The physical stress of hypertension on the arterial wall also results in the aggravation and acceleration of atherosclerosis, particularly of the coronary and cerebral vessels. Moreover, hypertension appears to increase the susceptibility of the small and large arteries to atherosclerosis.
The most likely cause of arterial thrombosis is artery damage due to atherosclerosis. Atherosclerosis occurs when a person has a buildup of plaque on the walls of their arteries. The arteries then begin to narrow and harden, which increases a person's risk of developing arterial thrombosis.
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
Ans: PHARMACOLOGICAL INTERVENTIONS
1. TAB. Dytor
mechanism: Through its action in antagonizing the effect of aldosterone, spironolactone inhibits the exchange of sodium for potassium in the distal renal tubule and helps to prevent potassium loss.
2. TAB. Acitrom
mechanism: Acenocoumarol inhibits the action of an enzyme Vitamin K-epoxide reductase which is required for regeneration and maintaining levels of vitamin K required for blood clotting
3. TAB. Cardivas
mechanism:Carvedilol works by blocking the action of certain natural substances in your body, such as epinephrine, on the heart and blood vessels. This effect lowers your heart rate, blood pressure, and strain on your heart. Carvedilol belongs to a class of drugs known as alpha and beta-blockers.
4. INJ. HAI S/C
MECHANISM:Regulates glucose metabolism
Insulin and its analogues lower blood glucose by stimulating peripheral glucose uptake, especially by skeletal muscle and fat, and by inhibiting hepatic glucose production; insulin inhibits lipolysis and proteolysis and enhances protein synthesis; targets include skeletal muscle, liver, and adipose tissue
5.TAB. Digoxin
mechanism:
Digoxin has two principal mechanisms of action which are selectively employed depending on the indication:
Positive Ionotropic: It increases the force of contraction of the heart by reversibly inhibiting the activity of the myocardial Na-K ATPase pump,
an enzyme that controls the movement of ions into the heart.
6. Hypoglycemia symptoms explained
7. Watch for any bleeding manifestations like Petechiae, Bleeding gums.
8. APTT and INR are ordered on a regular basis when a person is taking the anticoagulant drug warfarin to make sure that the drug is producing the desired effect.
3) What is the pathogenesis of renal involvement due to heart failure (cardio renal syndrome)? Which type of cardio renal syndrome is this patient?
Ans: *cardiorenal syndrome type 4 is seen in this patient.
4) What are the risk factors for atherosclerosis in this patient?
Ans: effect of hypertention
They can also impair blood vessels' ability to relax and may stimulate the growth of smooth muscle cells inside arteries. All these changes can contribute to the artery-clogging process known as atherosclerosis.
5) Why was the patient asked to get those APTT, INR tests for review?
Ans: APTT and INR are ordered on a regular basis when a person is taking the anticoagulant drug warfarin to make sure that the drug is producing the desired effect.
Here, an INR of 3-4.5 is recommended. Warfarin should be started in conjunction with heparin or low molecular weight heparin when the diagnosis of venous thromboembolism is confirmed, although local protocols may vary in their starting doses and titration schedule.
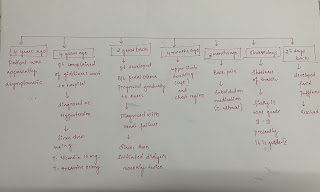
1)What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
TIMELINE OF EVENTS-
• Diabetes since 12 years - on medication
• Heart burn like episodes since an year- relieved without medication
• Diagnosed with pulmonary TB 7 months ago- completed full course of treatment, presently sputum negative.
• Hypertension since 6 months - on medication
• Shortness of breath since half an hour-SOB even at rest
Anatomical localisation - Cardiovascular system
Etiology: The patient is both Hypertensive and diabetic , both these conditions can cause
- Atherosclerosis: there is build up of fatty and fibrous material inside the wall of arteries.(PLAQUE)
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
Pharmacological interventions:
TAB MET XL 25 MG/STAT-contains Metoprolol as active ingredient
MOA: METOPROLOL is a cardiselective beta blocker
Beta blockers work by blocking the effects of the hormone epinephrine, also known as adrenaline. Beta blockers cause your heart to beat more slowly( negative chronotropic effect)
and with less force( negative inotropic effect). Beta blockers also help open up your veins and arteries to improve blood flow.
Indications: it is used to treat Angina, High blood pressure and to lower the risk of hear attacks .
EFFICACY STUDIES.
Patients were randomized to one of four treatment arms: placebo or ER metoprolol (0.2 mg/kg, 1.0 mg/kg, or 2.0 mg/kg). Data were analyzed on 140 intent-to-treat patients.
Results: mean baseline BP was 132/78 +/- 9/9 mmHg. Following 4 weeks of treatment, mean changes in sitting BP were: placebo = -1.9/-2.1 mmHg; ER metoprolol 0.2 mg/kg = -5.2/-3.1 mmHg; 1.0 mg/kg = -7.7/-4.9 mmHg; 2.0 mg/kg = -6.3/-7.5 mmHg. Compared with placebo, ER metoprolol significantly reduced systolic blood pressure (SBP) at the 1.0 and 2.0 mg/kg dose (P = .027 and P = .049, respectively), reduced diastolic blood pressure (DBP) at the 2.0 mg/kg dose (P = .017), and showed a statistically significant dose response relationship for the placebo-corrected change in DBP from baseline. There were no serious adverse events or adverse events requiring study drug discontinuation among patients receiving active therapy.
Non pharmacological intervention advised to this patient is: PERCUTANEOUS CORONARY INTERVENTION.
Percutaneous Coronary Intervention is a non-surgical procedure that uses a catheter (a thin flexible tube) to place a small structure called a stent to open up blood vessels in the heart that have been narrowed by plaque buildup ( atherosclerosis).
3) What are the indications and contraindications for PCI?
INDICATIONS:
Acute ST-elevation myocardial infarction (STEMI)
Non–ST-elevation acute coronary syndrome (NSTE-ACS)
Unstable angina.
Stable angina.
Anginal equivalent (eg, dyspnea, arrhythmia, or dizziness or syncope)
High risk stress test findings.
CONTRAINDICATIONS:
Intolerance for oral antiplatelets long-term.
Absence of cardiac surgery backup.
Hypercoagulable state.
High-grade chronic kidney disease.
Chronic total occlusion of SVG.
An artery with a diameter of <1.5 mm.
4) What happens if a PCI is performed in a patient who does not need it? What are the harms of overtreatment and why is research on overtesting and overtreatment important to current healthcare systems?
Although PCI is generally a safe procedure , it might cause serious certain complications like
A)Bleeding
B) Blood vessel damage
C) Allergic reaction to the contrast dye used
D) Arrhythmias
E) Need for emergency coronary artery bypass grafting .
Because of all these complications it is better to avoid PCI in patients who do not require it.
⁃ OVER TESTING AND OVER TRAETMENT HAVE BECOME COMMMIN IN TODAY’S MEDICAL PRACTICE.
⁃ Research on overtesting and overtreatment is important as they are more harmful than useful.
Harms to patients
. Performing screening tests in patients with who at low risk for the disease which is being screened.
For example:Breast Cancer Screenings Can Cause More Harm Than Good in Women Who Are at Low Risk. A harmless lump or bump could incorrectly come up as cancer during routine breast screenings. This means that some women undergo surgery, chemotherapy or radiation for cancer that was never there in the first place.
.Overuse of imaging techniques such as X- RAYS AND CT SCANS as a part of routine investigations.
Overuse of imaging can lead to a diagnosis of a condition that would have otherwise remained irrelevant - OVERDIAGNOSIS.
Also the adverse effects due to this are more when compared to the benefits.
.Overdiagnosis through overtesting can psychologically harm the patient.
Hospitalizations[41] for those with chronic conditions who could be treated as outpatients[ can lead to economic burden and a feeling of isolation.
Harms to health care systems
The use of expensive technologies and machineries are causing burden on health care systems.
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
Ans: *the anatomical location ofetiology is BLOOD VESSELS.
*myocardial infarction is usually due to thrombotic occlusion of a coronary vessel caused by rupture of a vulnerable plaque. Ischemia induces profound metabolic and ionic perturbations in the affected myocardium and causes rapid depression of systolic function
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
Ans: PHARMACOLOGICAL INNTERVENTION
1.TAB. ASPIRIN
mechanism:Aspirin inhibits platelet function through irreversible inhibition of cyclooxygenase (COX) activity. Until recently, aspirin has been mainly used for primary and secondary prevention of arterial antithrombotic events.
2.TAB ATORVAS
mechanism:Atorvastatin competitively inhibits 3-hydroxy-3-methylglutaryl-
3.TAB CLOPIBB
mechanism:The active metabolite of clopidogrel selectively inhibits the binding of adenosine diphosphate (ADP) to its platelet P2Y12 receptor and the subsequent ADP- mediated activation of the glycoprotein GPIIb/IIIa complex, thereby inhibiting platelet aggregation. This action is irreversible.
4.INJ HAI
mechanism:Regulates glucose metabolism
Insulin and its analogues lower blood glucose by stimulating peripheral glucose uptake, especially by skeletal muscle and fat, and by inhibiting hepatic glucose production; insulin inhibits lipolysis and proteolysis and enhances protein synthesis; targets include skeletal muscle, liver, and adipose tissue
5.ANGIOPLASTY
mechanism:Angioplasty, also known as balloon angioplasty and percutaneous transluminal angioplasty (PTA), is a minimally invasive endovascular procedure used to widen narrowed or obstructed arteries or veins, typically to treat arterial atherosclerosis.
3) Did the secondary PTCA do any good to the patient or was it unnecessary?
Ans:the second PCI was NOT necessary in this patient.
PCI performed from 3 to 28 days after MI does not decrease the incidence of death, reinfarction or New York Heart Association (NYHA) class IV heart failure but it is associated with higher rates of both procedure-related and true ST elevation reinfarction.3 A retrospective analysis of the clinical data revealed The Thrombolysis in Myocardial Infarction (TIMI) Risk Score of 4 predicting a 30-day mortality of 7.3% in this patient. Late PCI leads to the increased risks of periprocedural complications, long-term bleeding, and stent thrombosis.
The high incidence of CAD and the increasing need for PCI provides an opportunity to evaluate its appropriate use and highlight potential overuse. PCI is frequently reported to be overused and inappropriately recommended. Behnke et al defined overuse as ‘use of unnecessary care when alternatives may produce similar outcomes, resulting in a higher cost without increased value’.8Overuse causes a heavy financial burden on people living in countries, where fee-for-service and ill-regulated private healthcare provides much of the patient care. As a result, cost of healthcare increases and causes potential harm to the patients.
4) Gastroenterology (& Pulmonology) 10 Marks
A) Link to patient details:
A) Link to patient details:
QUESTIONS:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and
where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
Evolution of symptomatology
H5 years back-1st episode of pain abdomen and vomitings
Stopped taking alcohol for 3 years
1 year back 5 to 6 episodes of pain abdomen and vomitings after starting to drink alcohol again
20 days back increased consumption of toddy intake
Since 1 week pain abdomen and vomiting
Since 4 days fever constipation and burning micturition
Anatomical localisation: Pancreas and left lung
Alcohol and its metabolites produce changes in the acinar cells, which may promote
premature intracellular digestive enzyme activation thereby predisposing the gland to autodigestive injury.
Pancreatic stellate cells (PSCs) are activated directly by alcohol and its metabolites and also by
cytokines and growth factors released during alcohol-induced pancreatic necroinflammation.
Activated PSCs are the key cells responsible for producing the fibrosis of alcoholic chronic pancreatitis
2) What is the efficacy of drugs used along with other non pharmacological
treatment modalities and how would you approach this patient as a treating physician?
A) * Non pharmacological interventions : drains ( malecot & icd )
* Even i as a treating physician will follow the same approach
B) Link to patient details:
1) What is causing the patient's dyspnea? How is it related to pancreatitis?
ANSWER
the cause of dyspnea might be PLEURAL EFFUSION
2) Name possible reasons why the patient has developed a state of hyperglycemia.
ANSWER
*This hyperglycemia could thus be the result of a hyperglucagonemia secondary to stress
* the result of decreased synthesis and release of insulin secondary to the damage of pancreatic β-cells
* elevated levels of catecholamines and cortisol
3) What is the reason for his elevated LFTs? Is there a specific marker for Alcoholic Fatty Liver disease?
ANSWER
LFT are increased due to hepatocyte injury
*If the liver is damaged or not functioning properly, ALT can be released into the blood.
This causes ALT levels to increase.
A higher than normal result on this test can be a sign of liver damage.
*elevated alanine transaminase (ALT) and aspartate transaminase (AST),
usually one to four times the upper limits of normal in alcoholic fatty liver.
The reasons for a classical 2:1 excess of serum AST activity compared to serum
ALT activity in alcoholic hepatitis have been attributed to
(i) decreased ALT activity most likely due to B6 depletion in the livers of alcoholics
(ii) mitochondrial damage leading to increased release of mAST in serum.
4) What is the line of treatment in this patient?
ANSWER
Plan of action and Treatment:
Investigations:
✓ 24 hour urinary protein
✓ Fasting and Post prandial Blood glucose
✓ HbA1c
✓ USG guided pleural tapping
Treatment:
IVF: 125 mL/hr
• Inj PAN 40mg i.v OD
• Inj ZOFER 4mg i.v sos
• Inj Tramadol 1 amp in 100 mL NS, i.v sos
• Tab Dolo 650mg sos
• GRBS charting 6th hourly
• BP charting 8th hourly
1) What is the most probable diagnosis in this patient?
Differential Diagnosis:
Ruptured Liver Abscess.
Organized collection secondary to Hollow viscous Perforation.
Organized Intraperitoneal Hematoma.
Free fluid with internal echoes in Bilateral in the Subdiaphragmatic space.
Grade 3 RPD of right Kidney
The most probably diagnosis is there is abdominal hemorrhage. This will give reasoning to the abdominal
distention, and the blood which is aspirated.
2) What was the cause of her death?
After leaving the hospital, the patient went to Hyderabad and underwent an emergency laparotomy
surgery. The patient passed away the next day. Cause of her death can be due to complications of
laparotomy surgery such as, hemorrhage (bleeding), infection, or damage to internal organs.
3) Does her NSAID abuse have something to do with her condition? How?
NSAID-induced renal dysfunction has a wide spectrum of negative effects, including decreased
glomerular perfusion, decreased glomerular filtration rate, and acute renal failure. Chronic NSAIDs use
has also been related to hepatotoxicity. While the major adverse effects of NSAIDs such as
gastrointestinal mucosa injury are well known, NSAIDs have also been associated with hepatic side
effects ranging from asymptomatic elevations in serum aminotransferasevations levels and hepatitis with
jaundice to fulminant liver failure and death.
1.what could be the cause for his SOB
Ans- His sob was is due to Acidosis which was caused by Diuretics
2. Reason for Intermittent Episodes of drowsiness
Ans-Hyponatremia was the cause for his drowsiness
3.why did he complaint of fleshy mass like passage inurine
Ans-plenty of pus cells in his urine passage appeared as
fleshy mass like passage to him
4. What are the complicat ions of TURP that he may have had
Ans-
Difficulty micturition
Electrolyte imbalances
Infection
7) Infectious disease and Hepatology
1. Do you think drinking locally made alcohol caused
liver abscess in this patient due to predisposing factors
present in it ?
ANSWER
LIVER ABSSIS
yes, it could be due to intake of contaminated toddy
2. What is the etiopathogenesis of liver abscess in a chronic alcoholic patient ?
( since 30 years - 1 bottle per day)
2ans - according to some studies, alcoholism mainly consuming locally prepared
alcohol plays a major role as a predisposing factor for the formation of liver
abscesses that is both amoebic as well as pyogenic liver abscess
because of the adverse effects of alcohol over the Liver.
3. Is liver abscess more common in right lobe ?
ANSWER
Due to more blood sypply
4.What are the indications for ultrasound guided aspiration of liver abscess ?
ANSWER
1. Large abscess more than 6cms
2. Left lobe abscess
3.Caudate lobe abscess
4. Abscess which is not responding to drugs
1) Cause of liver abcess in this patient ?
A) Here ; the cause of liver abcess is :
* Amoebic liver abcess (ALA ) seen commonly in the tropics is predominantly confined to adult males,
especially those who consume locally brewed alcohol, although intestinal amoebiasis occurs in all age groups and in both genders.
* It has been argued that socioeconomic factors and poor sanitary conditions are the primary culprits that casually link alcohol to ALA.
* However , there has emerged an abundance of data that implicates alcohol in a more causal
role in facilitating the extraintestinal invasion of the infective protozoan and the subsequent development of ALA.
## Hence the consumption of locally made alcohol ( toddy ) is the most likely cause of Liver abcess in this patient.
2) How do you approach this patient ?
A) * The patient is well managed by treating team ; even me will follow the same approach.
3) Why do we treat here ; both amoebic and pyogenic liver abscess?
A) * Considering the following factors:
1) Age and gender of patient: 21 years ( young ) and male.
2) Single abcess.
3) Right lobe involvement.
## The abcess is most likely AMOEBIC LIVER ABSCESS …
** But most of the patients with amoebic liver abcess have no bowel symptoms, examination of stool
for ova and parasite and antigen testing is insensitive and insensitive and not recommended.
# And considering the risk factors associated with aspiration for pus culture:
1) Sometimes ; abcess is not accessible for aspiration if it is in posterior aspect or so.
2) Sometimes ; it has thin thinwall which may rupture if u aspirate.
3) Sometimes ; it is unliquefied.
## There how can u confirm whether it is pyogenic/ amoebic , so we treat them both empirically in clinical practice.
4) Is there a way to confirmthe definitive diagnosis in this patient?
A) There is no way to confirm the definitive diagnosis…(as mentioned above)
QUESTION: What is the evolution of the symptomatology in this patient in terms of an event
timeline and where is the anatomical localization for the problem and what is the primary
aetiology of the patient's problem?
1. 3 years ago- diagnosed with hypertension
2. 21 days ago- received vaccination at local PHC which was followed by fever
associated with chills and rigors, high grade fever, no diurnal variation which was
relieved on medication
3. 18 days ago- complained of similar events and went to the the local hospital, it was
not subsided upon taking medication(antipyretics)
4. 11 days ago - c/o Generalized weakness and facial puffiness and periorbital oedema.
Patient was in a drowsy state
5. 4 days ago-
a. patient presented to casualty in altered state with facial puffiness and
periorbital oedema and weakness of right upper limb and lower limb
b. towards the evening patient periorbital oedema progressed
c. serous discharge from the left eye that was blood tinged
d. was diagnosed with diabetes mellitus
6. patient was referred to a government general hospital
7. patient died 2 days ago
patient was diagnosed with diabetic ketoacidosis and was unaware that he was diabetic until
then. This resulted in poorly controlled blood sugar levels. The patient was diagnosed with
acute oro rhino orbital mucormycosis . rhino cerebral mucormycosis is the most common
form of this fungus that occurs in people with uncontrolled diabetes (
https://www.cdc.gov/fungal/diseases/mucormycosis/definition.html ) the fungus enters the
sinuses from the environment and then the brain.
The patient was also diagnosed with acute infarct in the left frontal and temporal lobe.
Mucormycosis is associated with the occurrence of CVA (
https://journal.chestnet.org/article/S0012-3692(19)33482-
8/fulltext#:~:text=There%20are%20few%20incidences%20reported,to%20better%20morbidit
y%2Fmortality%20outcomes. )
QUESTION: What is the efficacy of drugs used along with other non-pharmacological treatment
modalities and how would you approach this patient as a treating physician?
The proposed management of the patient was –
1. inj. Liposomal amphotericin B according to creatinine clearance
2. 200mg Iitraconazole was given as it was the only available drug which was
adjusted to his creatinine clearance
3. Deoxycholate was the required drug which was unavailable
https://pubmed.ncbi.nlm.nih.gov/23729001/ this article talks about the efficacy and toxicity of
different formulations of amphotericin B
along with the above mentioned treatment for the patient managing others symptoms is also
done by-
I. Management of diabetic ketoacidosis –
(a) Fluid replacement- The fluids will replace those lost through excessive
urination, as well as help dilute the excess sugar in blood.
(b) Electrolyte replacement-The absence of insulin can lower the level of
several electrolytes in blood. Patient will receive electrolytes through a
vein to help keep the heart, muscles and nerve cells functioning normally.
(c) Insulin therapy- Insulin reverses the processes that cause diabetic
ketoacidosis. In addition to fluids and electrolytes, patient will receive
insulin therapy
QUESTION: What are the postulated reasons for a sudden apparent rise in the
incidence of mucormycosis in India at this point of time?
Mucormycosis is may be being triggered by the use of steroids, a life-saving
treatment for severe and critically ill Covid-19 patients.
Steroids reduce inflammationin the lungs for Covid-19 and appear to help stop some of the damage that can
happen when the body's immune system goes into overdrive to fight off coronavirus.
But they also reduce immunity and push up blood sugar levels in both diabetics and
non-diabetic Covid-19 patients.
With the COVID-19 cases rising in India the rate of occurrence of mucormycosis in
these patients is increasing
Comments
Post a Comment