58 year old male with CKD on MHD.
"This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box
Chief complaints:
58 year old male, labourer by occupation, came to the OPD with the chief complaints of Shortness of breath since 15 days, worsened 3 days back, facial puffiness since 1 week.
History of Presenting illness -
Patient was apparently asymptomatic 4 years ago
4 years ago - pt complained of giddiness, went to a local hospital and was diagnosed as Hypertensive, on regular medication since then T. Nicardia 10mg, T. Arkamine 0.1mg sos
2 years back Pt developed B/L pedal edema, progressed gradually to knees, diagnosed with renal failure and initiated dialysis weekly twice
Left upper limb swelling, gradually progressing to current size, since 4 months . Swelling in the left chest region, gradually progressing to current size, since 4 months.
Back pain since 2 months, subsided on medication (T. Ultracet)
Shortness of breath since 45days
Grade II-III progressed to Grade IV since 15 days along with orthopnea .
27 days back - developed Facial puffiness
No c/o palpitations, giddiness, cold, cough, burning micturition.
PAST HISTORY -
Known case of Hypertension since 4years on Tab nifedipine 10mg OD
Not K/C/O TB, Epilepsy, Asthma, CAD.
Personal history:
He is a daily wage labourer , he goes to work in the morning and come in the evening. He used to drink toddy daily 1lit/ day since adulthood. Occasionally alcohol
After he got symptomatized , he used to go to work very lately and decrease in efficiency.
After diagnosed with hypertension, he stopped drinking toddy.
Appetite- normal
Diet- mixed
Bowel movement- Regular
Alcoholic stopped 4 yrs ago
Non smoker.
On examination:
Pt is C/c/c
No Pallor,Icterus,Cyanosis,Lymphadenopathy
Edema of feet + .
Vitals:
Pr:94bpm
Bp:130/90
Spo2:97% at RA
Temp - Afebrile
Today’s vitals:
BP:130/90
Pulse rate:95bpm
Spo2 -99% on 10ltrs of O2.
Systemic examination:
CVS - S1,S2 +
RS - BAE +
CNS - NAD
P/A- Soft, non tender.Investigations
Serology - Negative
Provisional Diagnosis -CKD on MHD.
Treatment:
Fluid restriction (<1l/day)
Salt restriction (<2g/day)
T· LASIX 40 mg PO BD.
T. Nicardia 100mg PO BD
T. NODOSIS 500 MG PO BD
T. OROFER-XR PO OD
T. SHELCAL-CT PO OD.
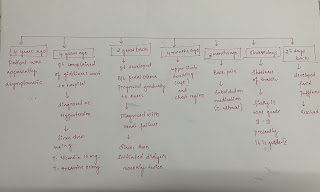
Clinical images:
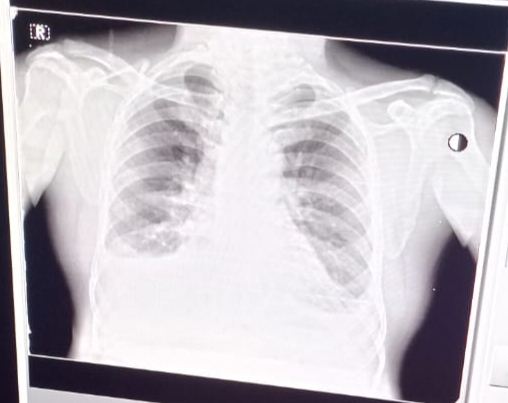
X rays:


















Comments
Post a Comment