22 year old female
This is an online E log book to discuss our patient's de-identified health data shared after taking her guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This E log book also reflects my patient-centered online learning portfolio.
CASE
22 year old female housewife resident of Nalgonda district came to OPD on 10th June 2022
With the chief complaints of
* generalized swelling of body since 5 days
* reduced urine output since 5 days
* shortness of breath since 5 days
HISTORY OF PRESENTING ILLNESS
Paitent was apparently asymptomatic 5 days ago then she had developed generalized swelling and reduced urine output
No complaints of palpitations, cold, cough, burning micturition fever,chest pain,
PAST HISTORY
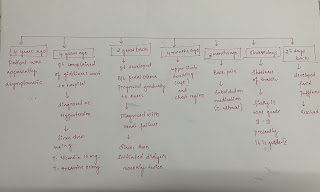
In 2010 when Paitent was 10 years old marked
*increased appetite
* increased urine output
*increased thirst
Were noted and she was taken to a local hospital where she was diagnosed with DIABETES and is on insulin therapy from then
In 2021
When she went to a regular check up she was diagnosed with hypertension from then she is on regular medication
* tablet Telma 40mg
*tablet Nicardia 20 mg
In May 2022
When she was 22 years old she had developed
*facial puffiness
*odema in feet
* shortness of breath
Grade IV
Where she was treated with dialysis and was send home
JUNE 2022(Presently)
after 15days of dialysis treatment Paitent had again developed
*generalized oedema
* reduced urine output
* loss of appetite
* vomiting
Paitent is a know case of
*diabetes melittus since past 12 years
*hypertension since 1 year
Not a know case of asthma epilepsy tuberculosis
PERSONAL HISTORY
appetite - reduced since 15 days
Diet - mixed
Bladder movements - reduced
Bowel movements - reduced
allergy - Not known
Addiction - NIL
ON EXAMINATION
Pallor present
NO
icterus
cyanosis
clubbing
lymphadenopathy
oedema present
VITALS
ON 14TH
PR 86 bpm
BP 180/100mm hg
RR 24 cpm
Spo2 97%
SYSTEMIC EXAMINATION
CVS: S1 S2 heard
No murmur heard
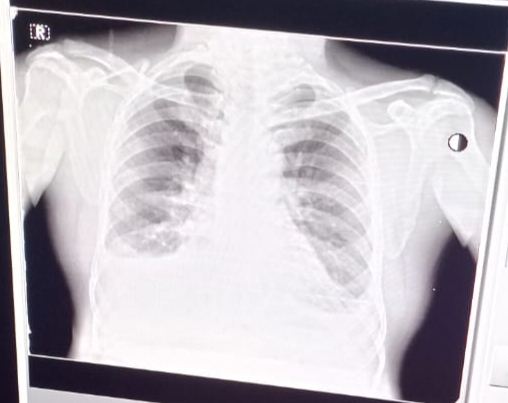
RS: bilateral crepitus heard
CNS: Crainial Nevers intact
Motor system intact
Sensory pain temp touch vibration well appreciated
Per Abdominal :
Inspection: distendent
Flanks full
Umbilicus center.
Palpation : soft and non tender
No organomegaly
Percussion fluid thrill present
DAIGONOSIS
CKD ON MHD
TREATMENT
Injection
PIPTAZ 2.25gm /TID/IV
PAN IV/BD
ZOFER IV/TID
Lasix 60 mg /BD
tablet
NICARDIA 20 MG /BD
TELMA 40 MG /OD
OROFER-X5 PO/OD
NODOSIS 500 MG PO/BD
SHELCAL 500MG/PO/OD









Comments
Post a Comment